Have you ever wondered why nearly every doctor's first recommendation for managing type 2 diabetes is weight loss? It's not about appearance or fitting into smaller clothes—it's about a profound biological transformation that occurs when we shed excess pounds. As someone who has guided thousands of patients through this journey, I've witnessed remarkable recoveries when people address the root cause rather than just managing symptoms.
The Fat-Insulin Connection You Need to Understand
When excess fat accumulates in your body—particularly visceral fat around your organs—it creates a cascade of metabolic disruptions. This isn't just passive storage tissue; it's biologically active, releasing inflammatory compounds and hormones that directly interfere with insulin function.
Here's what happens: As fat cells expand, they become stressed and inflamed, releasing cytokines (inflammatory messengers) that block insulin receptors throughout your body. Imagine putting the wrong key in a lock—insulin is present, but it can't open the door to let glucose enter your cells. The result? Your pancreas pumps out more and more insulin, desperately trying to overcome the resistance, while glucose remains trapped in your bloodstream.
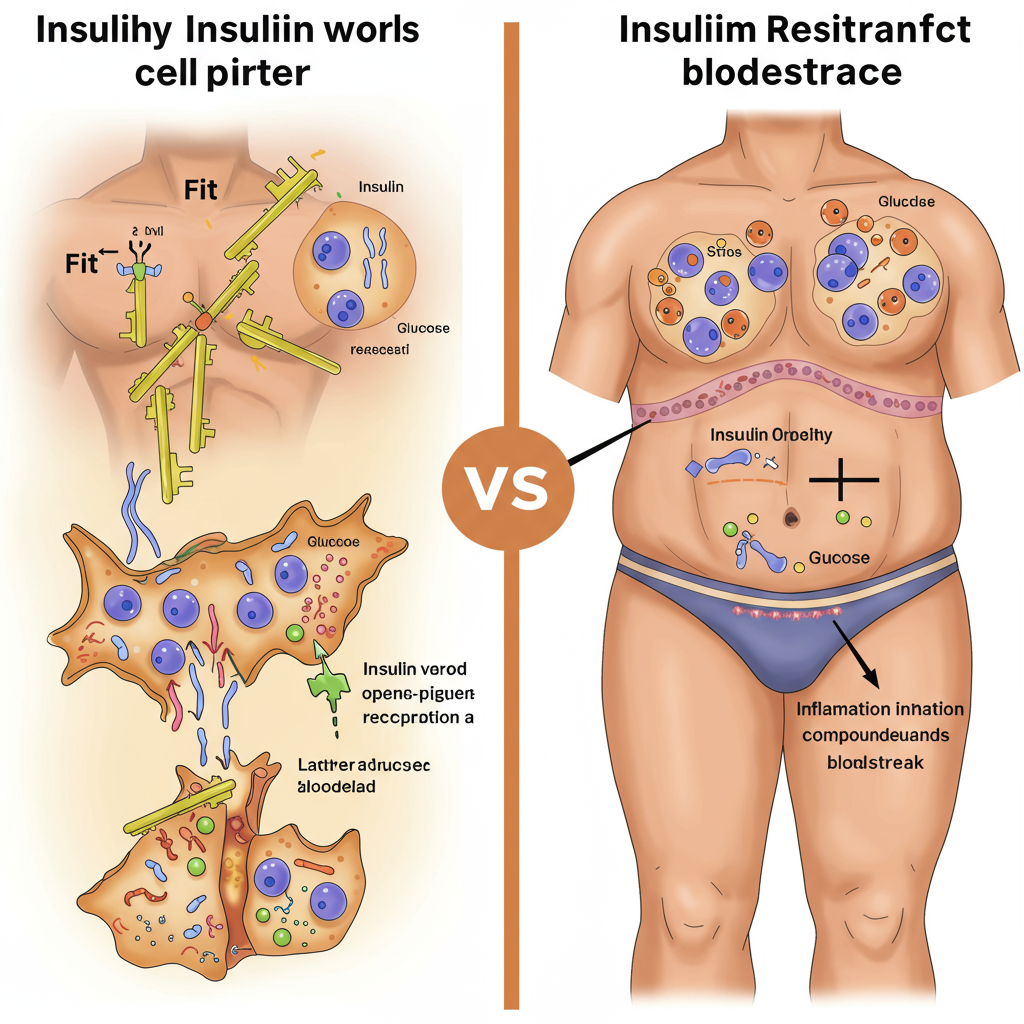
This condition—insulin resistance—is the precursor to type 2 diabetes, and it begins years before your blood sugar levels become noticeably elevated. The good news? This process is reversible, and weight loss is the most powerful intervention at our disposal.
The Metabolic Magic of Losing Just 5-10% of Body Weight
Many people believe they need to reach their "ideal body weight" to see health benefits, but the research tells a different story. Losing just 5-10% of your current weight can trigger significant metabolic improvements:
-
Immediate insulin sensitivity gains: Within days of beginning a calorie deficit, your body's insulin response begins to improve—even before significant weight loss occurs. This explains why many people see blood sugar improvements almost immediately after changing their diet.
-
Reduced liver fat: The liver plays a crucial role in glucose regulation. When you lose weight, one of the first places you lose fat is from your liver. Studies show that reducing liver fat rapidly improves insulin sensitivity and glucose metabolism.
-
Decreased inflammatory burden: Each pound of fat lost reduces the production of inflammatory compounds that interfere with insulin signaling, creating a virtuous cycle of improved metabolic health.
-
Enhanced mitochondrial function: Weight loss improves the function of mitochondria—your cells' energy factories—allowing them to burn glucose more efficiently rather than storing it as fat.

This explains why modest weight loss can lead to dramatic improvements in blood glucose levels, often reducing or eliminating the need for medication. I've seen patients reduce their HbA1c from diabetic ranges (above 6.5%) to completely normal levels (below 5.7%) with these changes.
The How Matters: Not All Weight Loss Approaches Are Created Equal
While any weight loss will likely improve blood sugar, how you lose the weight significantly impacts your long-term success. Here's what the research and my clinical experience show works best:
Focus on food quality, not just calories: Prioritize whole, unprocessed foods rich in fiber, healthy fats, and protein. These foods naturally regulate appetite while providing nutrients that support insulin sensitivity. Processed foods and refined carbohydrates, by contrast, trigger insulin spikes that promote fat storage and hunger.
Build muscle while losing fat: Resistance training preserves and builds muscle mass, which acts as a "glucose sink"—pulling sugar from your bloodstream even when insulin isn't working optimally. Aim for at least 2-3 strength training sessions weekly.
Address stress and sleep: Chronic stress and poor sleep directly elevate blood sugar and insulin resistance. Weight loss efforts that include stress management and sleep optimization yield better results than diet alone.
Consider intermittent fasting: Time-restricted eating (such as eating within an 8-10 hour window) has shown remarkable benefits for insulin sensitivity beyond its effects on weight loss. This approach gives your pancreas a much-needed rest and resets insulin receptors.
The most successful approach combines these elements rather than focusing solely on calorie restriction. This creates sustainable change that addresses the root causes of insulin resistance rather than just treating symptoms.

Conclusion: A Path Forward
Weight loss isn't simply about aesthetics—it's about creating fundamental biological changes that restore your body's natural ability to regulate blood sugar. By understanding this connection, you can approach weight management not as a cosmetic goal but as a powerful medical intervention.
If you're struggling with elevated blood sugar, know that you have more power to change your health trajectory than you might think. Small, consistent changes in diet, activity, and lifestyle can trigger profound metabolic improvements that medications alone cannot achieve.
Remember: your body wants to heal. Give it the right conditions, and it will.
References:
Taylor R. (2013). Type 2 diabetes: etiology and reversibility. Diabetes Care, 36(4), 1047-1055. https://doi.org/10.2337/dc12-1805
Magkos F, et al. (2016). Effects of Moderate and Subsequent Progressive Weight Loss on Metabolic Function and Adipose Tissue Biology in Humans with Obesity. Cell Metabolism, 23(4), 591-601. https://doi.org/10.1016/j.cmet.2016.02.005






