In the world of metabolic health, we often treat symptoms rather than root causes. Many weight loss programs focus on calories and willpower, but fail to address the metabolic dysfunction that drives weight gain in the first place. Today, I want to explore how continuous glucose monitoring (CGM) technology is revolutionizing weight management by providing real-time feedback on our metabolic responses.
The Glucose-Weight Connection: Why It Matters
When we talk about weight loss, we're typically focused on the wrong metrics. Counting calories matters, but what if your body's metabolic response to those calories varies dramatically based on food choices, timing, and other factors? This is where blood glucose comes into play.
Glucose—blood sugar—is our body's primary energy currency. When we eat carbohydrates or excess protein, blood glucose rises. In response, our pancreas secretes insulin, a powerful hormone with two critical functions: facilitating glucose entry into cells and promoting fat storage. This is a normal physiological process, but problems arise when this system becomes dysregulated.
Here's the inconvenient truth: chronically elevated insulin levels make weight loss nearly impossible. When insulin levels remain high, your body receives constant signals to store fat rather than burn it. Many people struggling with weight loss are caught in this metabolic trap without realizing it.
Traditional dietary advice often ignores individual glucose responses. Two people can eat identical meals and experience dramatically different glucose and insulin responses. One person might see their glucose rise to 160 mg/dL after eating a banana, while another might peak at only 110 mg/dL. These personalized responses explain why generic dietary recommendations fail so many people.
This is where CGM technology offers a breakthrough. Rather than guessing how foods affect you, a CGM provides continuous, real-time data on your personal glucose response. This feedback loop creates what behavioral scientists call "tight coupling"—an immediate connection between actions and outcomes that facilitates behavior change.
Using CGM Data to Guide Weight Loss Strategies
When you first start using a CGM, the data can be revelatory. Many people discover that foods they thought were healthy cause significant glucose spikes, while others learn that simple modifications can dramatically improve their metabolic response.
Here are key metrics to focus on for weight management:
-
Glucose variability: Aim to minimize large swings. The goal isn't necessarily a flat line but avoiding frequent, dramatic spikes above 140 mg/dL and crashes below 70 mg/dL.
-
Post-meal peaks: Ideally, blood glucose should return to baseline within 2-3 hours after eating. Persistent elevation suggests metabolic inefficiency.
-
Fasting glucose: Morning glucose between 70-90 mg/dL generally indicates good metabolic health.
-
Average glucose: An average below 100 mg/dL typically corresponds to healthy metabolic function.
The actionable insights from CGM data can transform your approach to nutrition:
Food composition and sequencing: Consuming fiber, fat, or protein before carbohydrates can blunt glucose spikes. For example, eating nuts before fruit or starting a meal with a salad before consuming starches.
Meal timing: Many people discover that their glucose regulation improves with time-restricted feeding (e.g., eating within an 8-10 hour window) and avoiding late-night eating.
Food substitutions: CGM data often reveals surprising individual responses to foods. Perhaps sweet potatoes spike your glucose but berries don't, or white rice causes problems while quinoa doesn't.
Exercise timing: A 20-minute walk after meals can reduce post-meal glucose peaks by 30-40% in many people, turning a problematic meal into an acceptable one.
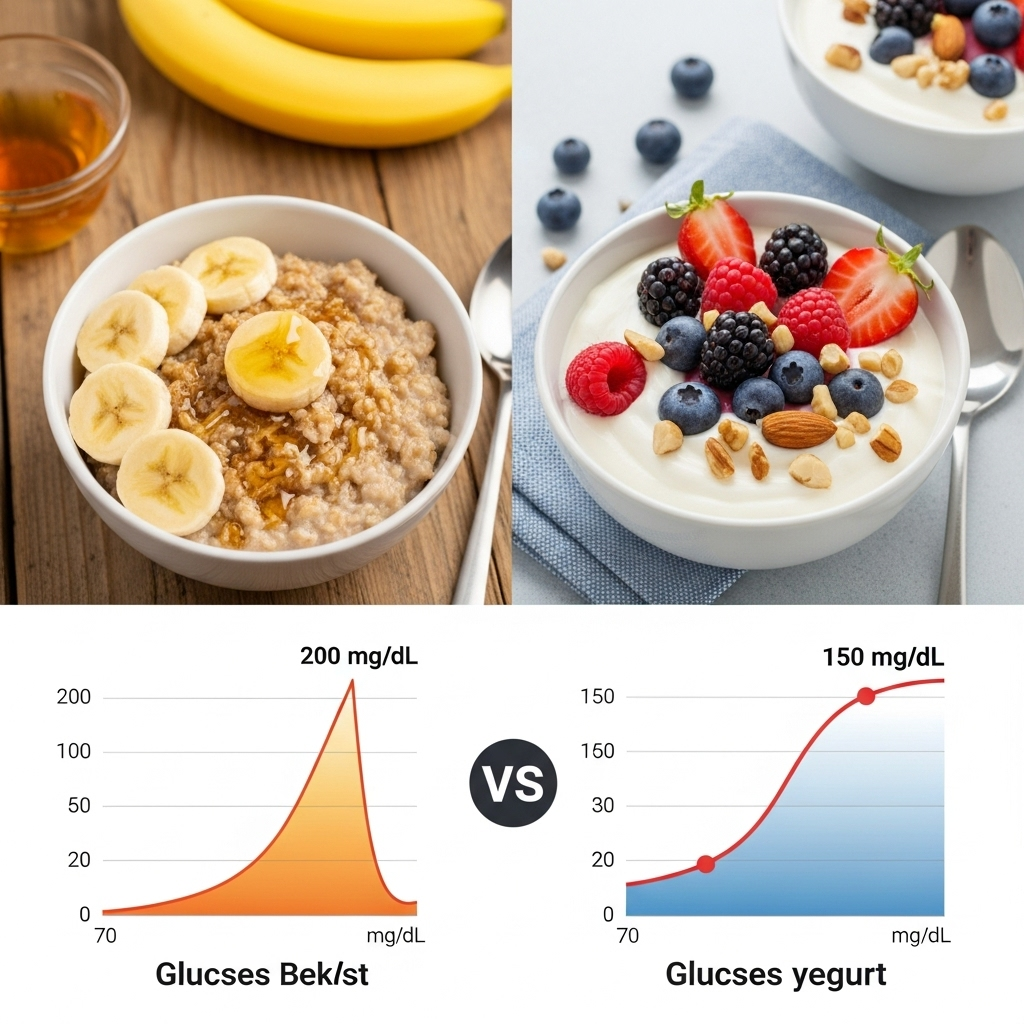
One patient of mine, Sarah, discovered through CGM data that her "healthy" breakfast of oatmeal with banana and honey was causing glucose spikes to nearly 180 mg/dL. By switching to Greek yogurt with berries and nuts, her morning peaks stayed under 110 mg/dL. This single change, driven by personal data rather than generic advice, helped break her weight loss plateau.
Beyond Food: The Glucose Impact of Lifestyle Factors
What makes CGM particularly valuable is its ability to capture how non-dietary factors affect your metabolism:
Sleep deprivation: Even one night of poor sleep can increase next-day glucose responses by 20-30% for the same meals. Many CGM users notice their worst glucose control follows their worst nights of sleep, creating a powerful incentive to prioritize sleep hygiene.
Stress management: Acute psychological stress triggers the release of cortisol and adrenaline, both of which can raise blood glucose independent of food intake. CGM users often observe glucose spikes during work presentations, difficult conversations, or even while watching suspenseful movies.
Physical activity patterns: Beyond structured exercise, CGM data reveals how simple movement throughout the day impacts glucose control. Many people discover that breaking up sedentary time with brief movement breaks (even just standing for phone calls) improves their daily glucose patterns.
Meal context: Eating the exact same meal in different contexts can produce different results. A meal consumed slowly and mindfully typically produces lower glucose peaks than the same meal eaten quickly while distracted.
These insights help people understand weight management as a comprehensive lifestyle approach rather than just a dietary challenge. When Sarah noticed her glucose running higher on stressful workdays, she implemented a brief meditation practice before meals, which measurably improved her postprandial glucose response.

Sustainability: The Missing Link in Weight Loss
The most valuable aspect of CGM-guided approaches may be their sustainability. Rather than relying on willpower to follow arbitrary rules, people make informed choices based on personalized data.
This creates several advantages:
-
Personalization over deprivation: Instead of avoiding all carbohydrates, you can identify which ones work for your metabolism and which don't.
-
Progress over perfection: CGM data shows that occasional indulgences don't derail metabolic health if they're balanced with strategies to minimize their impact.
-
Motivation through measurable progress: Improvements in glucose metrics often precede changes on the scale, providing early reinforcement that your efforts are working.
-
Data-driven course correction: When weight loss stalls, CGM data helps identify whether the issue is food choices, timing, stress, sleep, or other factors.
In clinical studies, people with access to glucose data typically achieve greater weight loss than those without it. One study found that prediabetic individuals using CGMs lost nearly twice as much weight as the control group, despite receiving the same dietary guidance. The real-time feedback appeared to improve both compliance and metabolic outcomes.
It's important to note that CGM is a tool for awareness, not a weight loss solution itself. The true power comes from using the data to guide sustainable lifestyle changes. And while CGMs were initially developed for diabetes management, their applications for metabolic health optimization extend to anyone concerned about weight management, energy levels, or long-term health.
Whether you're trying to lose 100 pounds or simply optimize your metabolic health, the personalized insights from continuous glucose monitoring can transform abstract nutritional concepts into concrete, actionable feedback. In a world of generic health advice, this level of personalization may be exactly what we need to finally address the epidemics of obesity and metabolic dysfunction.
References
-
Hall KD, Guo J. Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition. Gastroenterology. 2017;152(7):1718-1727. doi:10.1053/j.gastro.2017.01.052
-
Ranjan A, Schmidt S, Damm-Frydenberg C, et al. Short-term effects of a low-carbohydrate diet on glycaemic variables and cardiovascular risk markers in patients with type 1 diabetes: A randomized open-label crossover trial. Diabetes Obes Metab. 2017;19(10):1479-1484. doi:10.1111/dom.12953






