In my medical career, I've witnessed countless patients who were shocked to learn they had full-blown type 2 diabetes. Their most common refrain? "But I felt fine." This highlights one of the most dangerous aspects of metabolic dysfunction—it often progresses silently for years before causing noticeable symptoms. Today, I want to focus on prediabetes, the critical window of opportunity where intervention can dramatically alter your metabolic trajectory.
The Prediabetic State: More Than Just "Borderline" Diabetes
Prediabetes represents a metabolic warning sign—a state where blood glucose levels are elevated beyond healthy ranges but haven't yet reached diabetic thresholds. According to CDC statistics, over 96 million American adults (more than 1 in 3) have prediabetes, yet more than 80% don't know they have it.
What's happening physiologically? At its core, prediabetes typically stems from insulin resistance. Your pancreas produces insulin to help cells absorb glucose from your bloodstream. But when cells gradually become less responsive to insulin's signals, glucose builds up in the blood. Your pancreas responds by producing even more insulin, creating a vicious cycle.
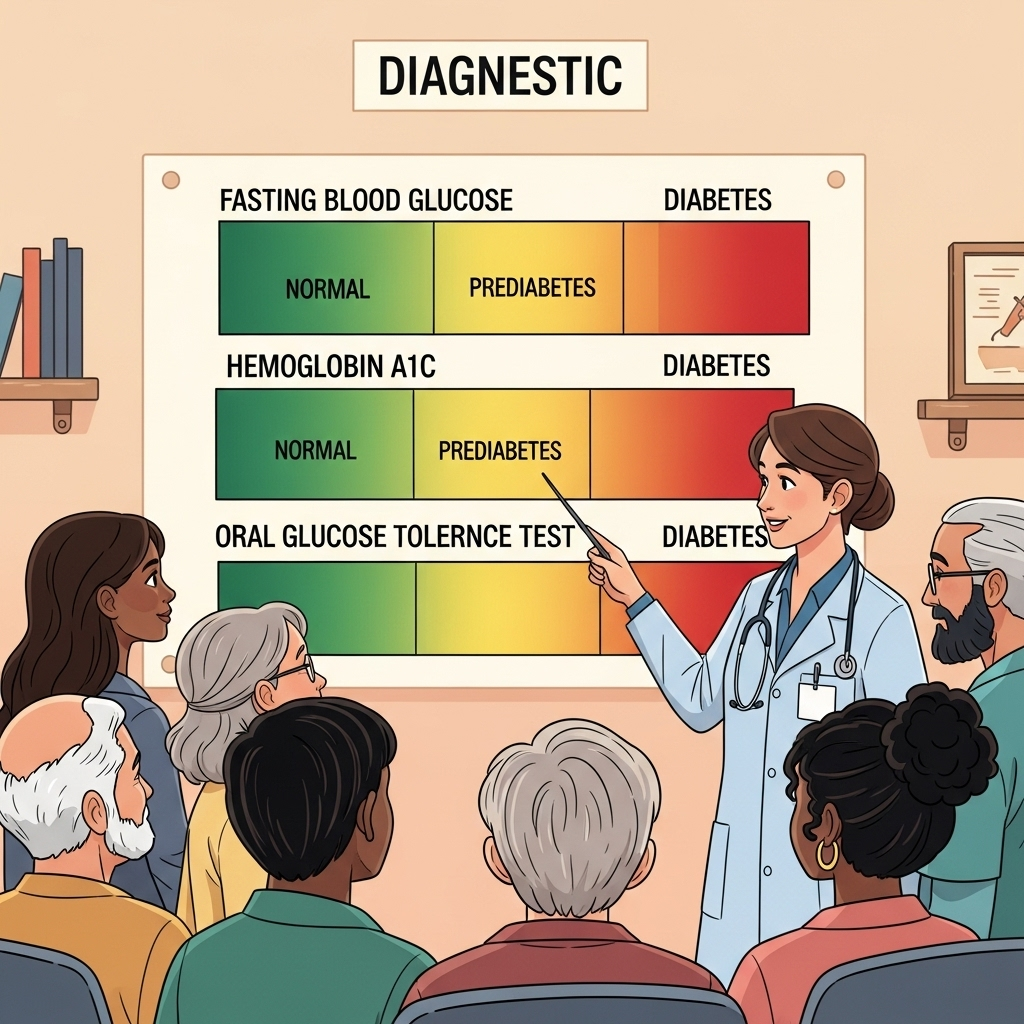
The diagnostic criteria are specific:
- Fasting blood glucose: Normal is below 100 mg/dL. Prediabetes falls between 100-125 mg/dL. At 126 mg/dL or higher, diabetes is diagnosed.
- Hemoglobin A1C: This measures your average blood sugar over approximately 3 months. Normal is below 5.7%, prediabetes is 5.7-6.4%, and diabetes is 6.5% or higher.
- Oral glucose tolerance test: After consuming a standardized glucose drink, your blood is tested. Readings between 140-199 mg/dL at the 2-hour mark indicate prediabetes.
What many people don't realize is that even "high-normal" ranges can signal trouble. If your fasting glucose consistently registers between 90-99 mg/dL, or your A1C hovers around 5.5-5.6%, you're not in the clear. These levels already indicate metabolic strain and increased long-term risk.
Beyond the Numbers: Who's at Risk?
Certain factors significantly increase your likelihood of developing prediabetes:
-
Weight status: Being overweight or obese, especially with abdominal fat (the dangerous "visceral fat" surrounding organs), dramatically increases risk. A waist circumference over 40 inches for men or 35 inches for women is particularly concerning.
-
Age: While type 2 diabetes is increasingly diagnosed in younger populations, risk still increases substantially after age 45.
-
Cardiovascular markers: High blood pressure (≥130/80 mmHg), elevated triglycerides (≥150 mg/dL), or low HDL cholesterol (<40 mg/dL for men, <50 mg/dL for women) often travel alongside insulin resistance.
-
Lifestyle factors: Physical inactivity is a major contributor. The human body wasn't designed for sedentary living—it thrives on movement.
-
Genetic predisposition: Family history matters. If a first-degree relative has type 2 diabetes, your risk increases substantially.
-
Pregnancy history: Women who developed gestational diabetes during pregnancy have a 7-fold increased risk of developing type 2 diabetes later.
-
Ethnic background: Hispanic/Latino, African American, Native American, and Asian American populations show higher predisposition to insulin resistance.
-
Sleep problems: Poor sleep quality, sleep apnea, and shift work all disrupt normal metabolic functioning.
The convergence of multiple risk factors creates a compounding effect. But here's the good news: identifying your risk profile early allows for targeted intervention, potentially preventing progression to diabetes altogether.
The Intervention Toolkit: Evidence-Based Approaches
The Diabetes Prevention Program, a landmark NIH study, demonstrated that lifestyle intervention reduced diabetes incidence by 58% compared to placebo—outperforming even medication (metformin, which reduced incidence by 31%). Here's how to implement evidence-based strategies:
1. Physical Activity: Beyond Just Burning Calories
Aerobic exercise improves insulin sensitivity acutely, with effects lasting 24-48 hours. This means consistent activity is crucial—aim for 150 minutes of moderate-intensity exercise weekly, ideally spread across at least 3 days with no more than 2 consecutive days without activity.
Strength training deserves special attention. Skeletal muscle is your body's primary site for glucose disposal. By building muscle mass through resistance training 2-3 times weekly, you're essentially expanding your "glucose sink"—the tissue that can effectively clear sugar from your bloodstream.

HIIT (High-Intensity Interval Training) has shown remarkable efficiency in improving insulin sensitivity. Even 10-20 minutes of HIIT can produce metabolic benefits comparable to longer moderate sessions, making it ideal for time-constrained individuals.
2. Nutritional Approach: Beyond Calorie Counting
Diet quality matters tremendously. Focus on:
-
Reducing refined carbohydrates and added sugars: These cause rapid glucose and insulin spikes, exactly what we're trying to avoid. This doesn't mean eliminating all carbohydrates—rather, choose complex carbs with fiber (vegetables, berries, legumes) over refined options.
-
Moderating protein intake: Aim for 1.6-2.2g per kg of ideal body weight daily, emphasizing high-quality sources (eggs, fish, poultry, legumes).
-
Embracing healthy fats: Contrary to outdated advice, quality fats from olive oil, avocados, nuts, and fatty fish don't cause insulin resistance—they often improve it.
-
Timing matters: Our glucose tolerance deteriorates throughout the day. A carbohydrate-heavy dinner typically produces a much larger glucose excursion than the exact same meal consumed at breakfast. Consider "front-loading" carbs earlier in the day.
-
Consider time-restricted feeding: Limiting your eating window to 8-10 hours daily (e.g., eating only between 9am-7pm) has shown promise in improving insulin sensitivity, even without calorie reduction.
3. Weight Management: Quality Over Quantity
While weight loss of just 5-7% of body weight can significantly reduce diabetes risk, how you lose weight matters. Crash diets that rely on extreme calorie restriction often backfire metabolically.
Focus instead on creating sustainable habits that lead to gradual weight reduction, particularly addressing visceral fat. The combination of resistance training and moderate caloric deficit produces the most favorable body composition changes, preserving muscle while reducing fat stores.
4. Tracking Progress: Beyond the Scale
Improvement begins within weeks of lifestyle changes, but the most substantial glycemic improvements typically occur within the first year of sustained change. How can you track progress?
- Regular testing: If you're prediabetic, consider checking A1C every 3-6 months.
- Monitor trends: Even within "normal" ranges, an A1C that's risen from 5.2% to 5.6% over two years signals deteriorating glucose control.
- Consider a continuous glucose monitor (CGM): These devices provide real-time feedback on how specific foods and activities affect your glucose levels, enabling personalized adjustments.
- Track biomarkers beyond glucose: Improvements in blood pressure, triglycerides, and inflammatory markers often accompany enhanced insulin sensitivity.
Conclusion: The Window of Opportunity
Prediabetes represents both a warning and an opportunity. Unlike fully established type 2 diabetes, which often requires medication to manage, prediabetes can frequently be reversed through lifestyle intervention alone.
The goal isn't perfection—it's progress. Small, consistent improvements compound over time. A daily 20-minute walk, replacing sugary beverages with water, prioritizing sleep, or adding a weekly strength training session might seem insignificant in isolation. But collectively, these habits can literally rewrite your metabolic future.
Don't wait for symptoms to appear—they rarely do until significant damage has occurred. If you haven't had your glucose levels checked recently, especially if you have risk factors, scheduling that screening could be the most important preventive health measure you take this year.

References:
-
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403. doi:10.1056/NEJMoa012512
-
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279-2290. doi:10.1016/S0140-6736(12)60283-9






