The Silent Destroyer: How Chronic High Blood Sugar Damages Your Body
Living with diabetes isn't just about managing blood glucose numbers on a meter. Those elevated glucose levels, when persistent over months and years, trigger a cascade of harmful effects throughout the body. Understanding this connection between high blood sugar and diabetes complications is crucial for anyone looking to prevent the serious consequences of this disease.
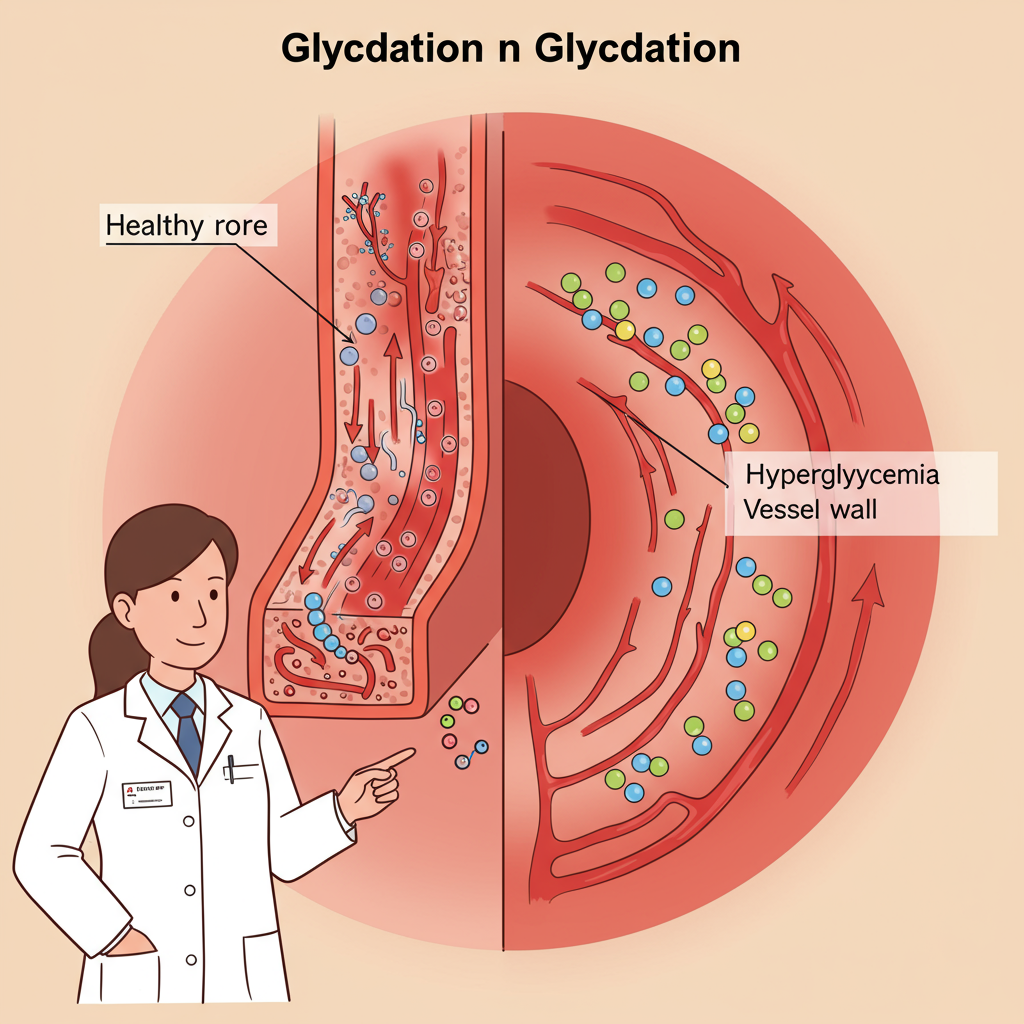
The Glucose Tsunami: How Hyperglycemia Damages Blood Vessels
When blood glucose remains chronically elevated—a condition we call hyperglycemia—it essentially bathes every blood vessel and organ in a solution that's more concentrated than it should be. This excess glucose doesn't just float around harmlessly. It chemically attaches to proteins in your blood vessels and tissues through a process called glycation, forming advanced glycation end products (AGEs).
These AGEs are troublemakers. They create cross-links in collagen (making tissues stiff), trigger inflammation, and cause oxidative stress. Your blood vessels, from the largest arteries to the tiniest capillaries, become damaged. The delicate endothelial lining—that single-cell barrier between your blood and vessel walls—becomes dysfunctional, setting the stage for atherosclerosis and microvascular disease.
What's particularly concerning is that this damage often begins years before diabetes is diagnosed. By the time many people learn they have diabetes, the vascular damage is already underway, affecting vital organs with rich blood supplies like the kidneys, eyes, and nerves.
Metabolic Memory: Why Early Control Matters
Perhaps one of the most fascinating and important concepts in diabetes management is what researchers call "metabolic memory" or the "legacy effect." This phenomenon refers to the lasting impact of early blood glucose control on long-term outcomes.
Large-scale studies like the Diabetes Control and Complications Trial (DCCT) and its follow-up, the Epidemiology of Diabetes Interventions and Complications (EDIC) study, have shown something remarkable: the benefits of tight glucose control early in the disease course persist for decades, even if control becomes less stringent later on. Conversely, early poor control creates a "negative memory" that increases complication risk down the road.

This metabolic memory likely occurs because hyperglycemia triggers epigenetic changes—modifications to how your genes are expressed without altering the DNA sequence itself. These changes can persist long after glucose levels are brought under control.
The implications are profound: the damage from high blood sugar isn't just about what your glucose is doing today—it's about the cumulative effect of every high and low over time, with early years having outsized importance.
The Organ Battlegrounds: Where Complications Strike
When we talk about diabetes complications, we're really discussing how hyperglycemia impacts specific organs and systems:
Kidneys (Nephropathy): The kidneys filter your blood through millions of tiny filtering units called glomeruli. High glucose damages these filters, causing them to leak protein into the urine. Over time, this leads to declining kidney function and potentially kidney failure requiring dialysis or transplantation.
Eyes (Retinopathy): The retina contains a network of delicate blood vessels that can weaken, bulge, and leak when damaged by high glucose. New, fragile blood vessels may grow abnormally (proliferative retinopathy), leading to vision loss or blindness if untreated.
Nerves (Neuropathy): High glucose damages nerves through direct metabolic effects and by impairing the tiny blood vessels that supply them. This typically begins as numbness, tingling, or pain in the extremities but can progress to affect autonomic functions like digestion, sexual response, and even heart rate regulation.
Heart and Blood Vessels (Cardiovascular Disease): People with diabetes have 2-4 times higher risk of heart attacks and strokes. Hyperglycemia accelerates atherosclerosis (hardening and narrowing of arteries), impairs circulation, and often coexists with hypertension and dyslipidemia—creating the perfect storm for cardiovascular events.
Breaking the Cycle: Strategies Beyond Glucose Control
While tight glucose control is foundational, a comprehensive approach to preventing complications includes:
-
Aggressive blood pressure management: Often as important as glucose control for preventing complications, especially for the kidneys and eyes.
-
Lipid optimization: Addressing the common pattern of high triglycerides and low HDL seen in diabetes.
-
Regular screening: Early detection of complications through kidney function tests, eye exams, foot checks, and cardiovascular assessments allows for intervention before damage becomes irreversible.
-
Novel therapies: Newer medication classes like SGLT-2 inhibitors and GLP-1 receptor agonists not only improve glucose control but appear to have direct protective effects on the kidneys and cardiovascular system.
-
Lifestyle fundamentals: Nutrition, physical activity, stress management, and sleep quality all influence both glucose control and the body's resilience against hyperglycemia-induced damage.

The relationship between high blood sugar and complications isn't simple or linear. Individual susceptibility varies tremendously, with some people developing complications despite reasonable control, while others remain complication-free despite suboptimal numbers. Genetics, environmental factors, and other health conditions all play roles in this complex equation.
What remains clear, however, is that consistently elevated blood glucose sets the stage for the most serious consequences of diabetes. Understanding this connection empowers us to take the right actions today that will protect our future health.
References:
-
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589. doi:10.1056/NEJMoa0806470
-
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615-1625. doi:10.2337/diabetes.54.6.1615






