Timing Matters: How Your Body Clock Influences Blood Sugar Control
For people with diabetes, managing blood sugar levels is a daily priority. But have you ever noticed that your glucose readings follow certain patterns throughout the day? Or that your blood sugar might react differently to the same meal depending on when you eat it? The explanation may lie in your body's internal clock—your circadian rhythm.
What Is Circadian Rhythm and How Does It Work?
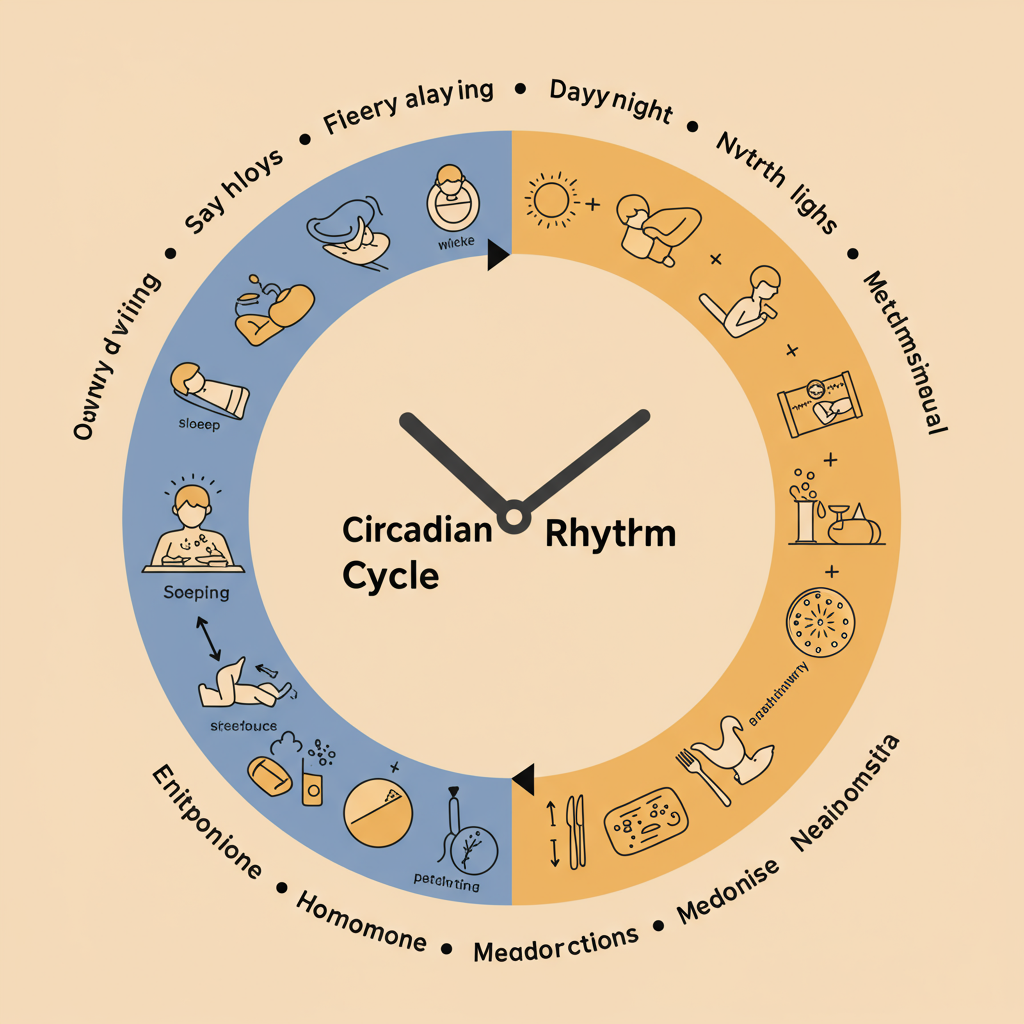
Your circadian rhythm is essentially a 24-hour internal clock that regulates numerous biological processes, including sleep-wake cycles, hormone release, body temperature, and—critically for people with diabetes—metabolism and blood glucose regulation.
This intricate system is primarily controlled by the suprachiasmatic nucleus (SCN), a tiny region in your brain's hypothalamus. The SCN receives light signals from your eyes and coordinates various body functions accordingly. When functioning properly, your circadian rhythm helps ensure that your body's processes occur at optimal times throughout the day.
For example, in people without diabetes, insulin sensitivity and glucose tolerance naturally fluctuate throughout the day. Most people experience peak insulin sensitivity in the morning and decreased sensitivity in the evening and night—a pattern that has evolved to match our traditional eating and activity schedules.
How Circadian Rhythm Affects Blood Glucose Levels
The relationship between circadian rhythm and blood glucose regulation is complex and bidirectional. Here's how your internal clock influences blood sugar control:
Hormone fluctuations: Your body naturally releases more cortisol (a stress hormone that raises blood sugar) in the early morning hours—often referred to as the "dawn phenomenon." This explains why many people with diabetes experience higher fasting glucose levels in the morning, even without eating.
Insulin sensitivity: Your cells' responsiveness to insulin follows a daily pattern. Research shows that the same meal consumed at breakfast typically produces a lower blood glucose response than when eaten at dinner, partly because insulin sensitivity is generally higher earlier in the day.
Melatonin production: The sleep hormone melatonin, which increases in the evening, can temporarily reduce insulin secretion. This means late-night snacking may cause higher blood sugar spikes than eating the same foods earlier in the day.
Glucose metabolism in the liver: Your liver's production and storage of glucose follows circadian patterns, with increased glucose output during the night and early morning to ensure your brain has energy while you sleep.
Practical Implications for Diabetes Management

Consistent meal timing: Try to eat meals at similar times each day to help maintain a stable circadian rhythm. Your body anticipates food at regular intervals and prepares accordingly by releasing appropriate hormones.
Earlier meals may be better: Consider consuming your largest meals earlier in the day when insulin sensitivity is typically higher. Some studies suggest that front-loading your calories (eating a substantial breakfast and lighter dinner) may improve glucose control.
Regular sleep schedule: Aim for 7-8 hours of quality sleep and maintain consistent sleep and wake times. Poor sleep or irregular sleep patterns can disrupt your circadian rhythm and impair insulin sensitivity.
Light exposure management: Get bright light exposure in the morning to help reinforce your circadian rhythm, and limit blue light from screens in the evening when your body should be preparing for sleep.
Medication timing: Work with your healthcare provider to time your diabetes medications appropriately. For instance, some people may need higher insulin doses or different basal insulin rates during the early morning to counteract the dawn phenomenon.
When Circadian Rhythm Gets Disrupted
Modern life doesn't always align with our biological clocks. Shift work, jet lag, irregular sleep patterns, and even seasonal changes can disrupt circadian rhythms and potentially worsen blood glucose control.
Research has shown that chronic circadian disruption is associated with increased risk of type 2 diabetes and poorer outcomes in people who already have diabetes. Shift workers, who regularly experience circadian misalignment, have approximately a 40% higher risk of developing type 2 diabetes compared to day workers.
If your schedule requires activities that might disrupt your circadian rhythm, work closely with your healthcare team to develop strategies that minimize the impact on your blood glucose management.
Understanding the powerful influence of your body's internal clock on blood sugar regulation adds another dimension to diabetes self-management. By aligning your daily habits with your natural circadian rhythm whenever possible, you may discover a valuable tool for achieving more stable blood glucose levels throughout the day.
References:
Mason IC, Qian J, Adler GK, Scheer FAJL. Impact of circadian disruption on glucose metabolism: implications for type 2 diabetes. Diabetologia. 2020;63(3):462-472.
Qian J, Scheer FAJL. Circadian System and Glucose Metabolism: Implications for Physiology and Disease. Trends in Endocrinology & Metabolism. 2016;27(5):282-293.






