The Mind-Glucose Connection: How Mindfulness Practices May Help Regulate Blood Sugar
In the world of diabetes management, we often focus on the obvious factors: diet, exercise, medication, and insulin. But there's another powerful tool that deserves our attention—the practice of mindfulness and meditation. As someone who regularly explores the intersection of neuroscience and health, I find the emerging research on how our mental states affect physiological processes like blood glucose regulation particularly fascinating.
The Stress-Blood Sugar Connection
When we experience stress, our bodies initiate the "fight or flight" response, triggering the release of hormones like cortisol and adrenaline. These hormones serve an evolutionary purpose: they prepare our bodies to respond to threats by mobilizing energy resources—specifically, glucose—into the bloodstream.
For our ancestors facing physical threats, this glucose surge would be quickly utilized through intense physical activity. However, in our modern world, stress is often psychological rather than physical. When we experience chronic stress without the corresponding physical exertion, these elevated blood glucose levels can remain high, creating particular challenges for people with diabetes.
This is where the science of mindfulness comes in. Mindfulness practices have been shown to significantly reduce stress hormone production, potentially mitigating these unwanted blood glucose elevations.

The Science Behind Mindfulness and Blood Sugar
Research has begun to illuminate how mindfulness practices might directly influence glycemic control. A systematic review published in the Journal of Diabetes Research found that mindfulness-based interventions were associated with significant reductions in fasting blood glucose and HbA1c levels in people with type 2 diabetes.
The mechanisms appear to be multifaceted:
-
Stress Reduction: By lowering cortisol levels, mindfulness practices may reduce insulin resistance and improve glucose uptake by cells.
-
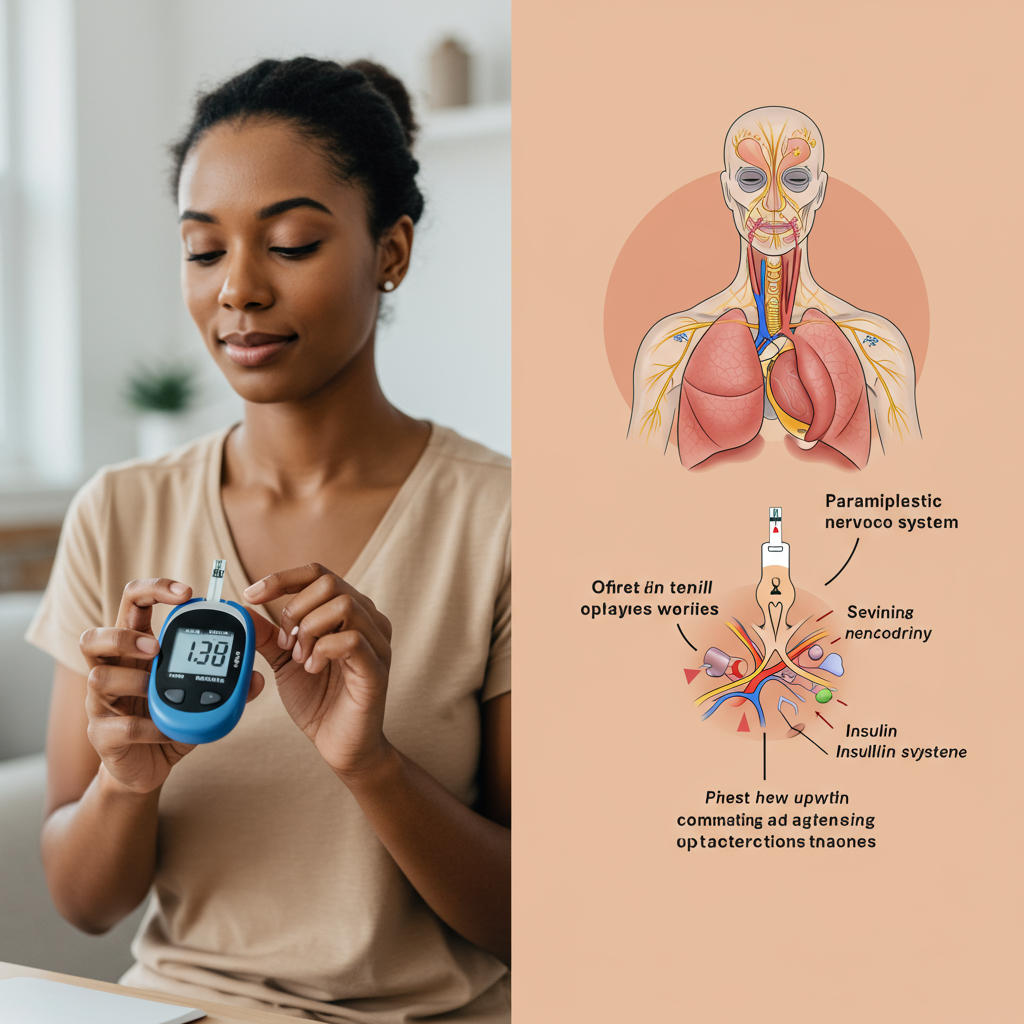
Autonomic Nervous System Regulation: Meditation shifts the body from sympathetic ("fight or flight") dominance toward parasympathetic ("rest and digest") activity, which may improve metabolic function.
-
Improved Sleep Quality: Mindfulness improves sleep, which is essential for proper glucose metabolism and insulin sensitivity.
-
Enhanced Body Awareness: Regular mindfulness practice increases interoception—awareness of internal bodily sensations—which may help people make better dietary and lifestyle choices.
What's particularly interesting from a neuroscientific perspective is that these effects aren't just psychological; they represent real, measurable changes in physiological function that can be observed in laboratory settings.
Implementing Mindfulness for Blood Sugar Management
If you're interested in exploring mindfulness as a complementary approach to blood sugar management, here are some evidence-informed practices to consider:
Breathing Exercises: Even 5-10 minutes of deep, diaphragmatic breathing can trigger your parasympathetic nervous system, potentially reducing stress-induced glucose elevations. Try a simple 4-4-4-4 pattern: inhale for 4 seconds, hold for 4, exhale for 4, and pause for 4 before repeating.
Body Scan Meditation: This practice involves systematically bringing attention to different parts of your body, noticing sensations without judgment. Research suggests this may improve insulin sensitivity over time.
Mindful Eating: By paying full attention to the experience of eating—textures, flavors, aromas, and physical sensations—you may improve digestion and metabolic response to food. Additionally, this practice often leads to better food choices and appropriate portion sizes.
Consistent Practice: Like physical exercise, consistency matters more than duration. A daily 10-minute practice will likely yield better results than an occasional hour-long session.

For those managing diabetes, I recommend tracking your blood glucose before and after mindfulness sessions over several weeks. This personal data can help you identify which practices are most effective for your unique physiology.
Conclusion: A Complementary Approach
It's important to emphasize that mindfulness should complement, not replace, conventional diabetes care. The most powerful approach integrates proper medical management with lifestyle optimization, including mindfulness practices.
What makes this area particularly exciting is that mindfulness represents a no-cost intervention with virtually no side effects, but potentially significant benefits. As research continues to evolve, we're gaining a deeper understanding of the profound connections between our mental states and metabolic health.
By incorporating these practices into your daily routine, you may discover not only better blood glucose control but also improvements in overall well-being, sleep quality, and stress management—benefits that extend far beyond diabetes care alone.
References:
Kiran, Y., & Prakash, S. (2019). Effect of Mindfulness-Based Stress Reduction Program on Stress, Anxiety, Depression and Glycemic Control in Type 2 Diabetes Mellitus: A Systematic Review. Journal of Diabetes Research, 2019, 6981483. https://doi.org/10.1155/2019/6981483
Rosenzweig, S., Reibel, D. K., Greeson, J. M., Edman, J. S., Jasser, S. A., McMearty, K. D., & Goldstein, B. J. (2007). Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Alternative Therapies in Health and Medicine, 13(5), 36-38.






