Living with Diabetes: Understanding the Critical Differences Between Type 1 and Type 2
Diabetes has become one of the most prevalent chronic conditions globally, affecting hundreds of millions of people. Yet despite its widespread nature, confusion persists about the different types of diabetes and their distinct characteristics. In this post, we'll clarify the essential differences between Type 1 and Type 2 diabetes, helping you understand their unique causes, symptoms, and treatment approaches.
What Is Diabetes?
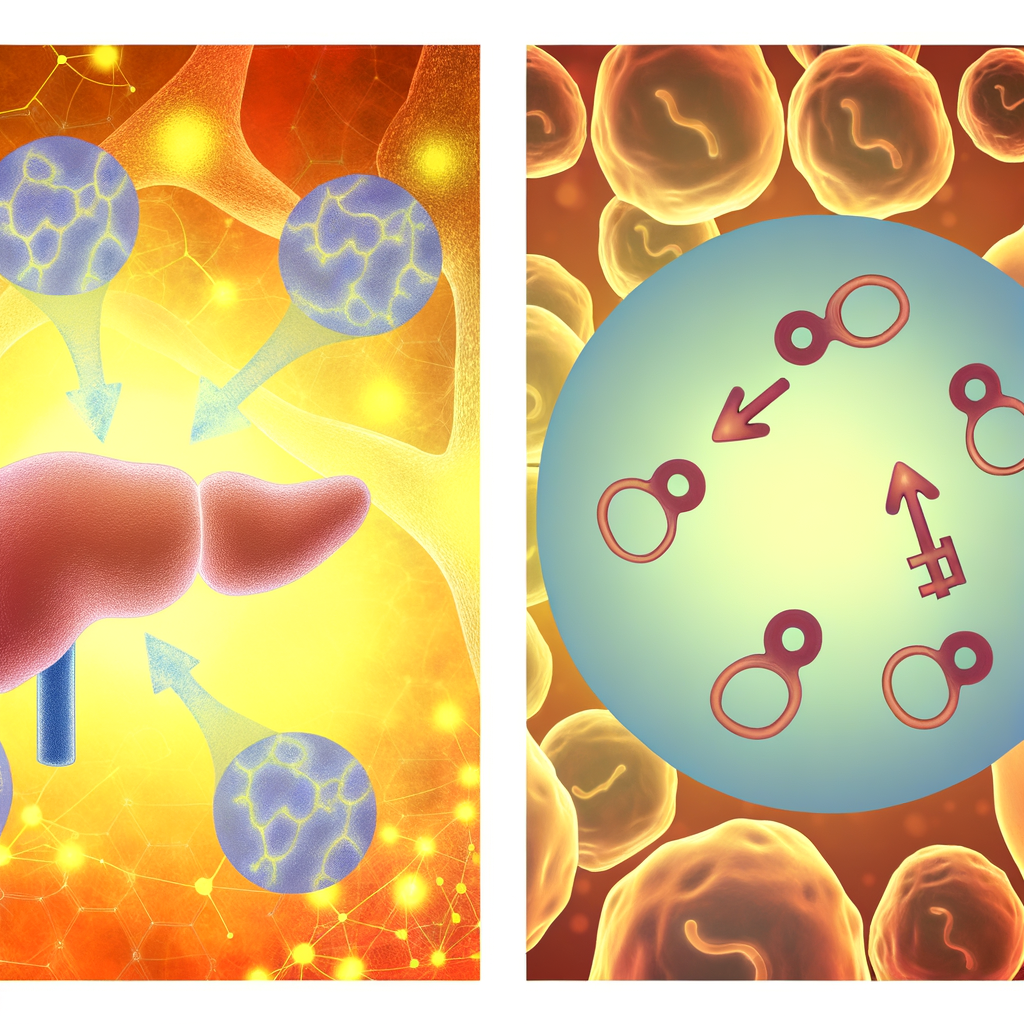
At its core, diabetes is a group of metabolic disorders characterized by high blood glucose (sugar) levels that result from defects in insulin production, insulin action, or both. Insulin, a hormone produced by the pancreas, helps move glucose from the bloodstream into cells to be used for energy.
Type 1 Diabetes: The Autoimmune Variant
Cause and Mechanism
Type 1 diabetes results from an autoimmune response where the body's immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This attack leaves the body with little to no ability to produce insulin naturally.
Who It Affects
Type 1 diabetes accounts for approximately 5-10% of all diabetes cases and is usually diagnosed in children, adolescents, or young adults, although it can develop at any age. Due to its common onset in younger individuals, it was previously called "juvenile diabetes."
Key Symptoms
The onset of Type 1 diabetes is typically rapid and symptoms can be severe:
- Extreme thirst and frequent urination
- Unexplained weight loss despite increased appetite
- Fatigue and weakness
- Blurred vision
- Irritability and mood changes
Treatment Approach
Since Type 1 diabetics cannot produce insulin, the primary treatment involves:
- Insulin therapy: Required for survival, delivered via multiple daily injections or an insulin pump
- Blood glucose monitoring: Regular testing throughout the day
- Carbohydrate counting: Matching insulin doses to carbohydrate intake
- Regular physical activity: To help manage blood glucose levels
- Healthy eating: Focusing on consistent carbohydrate intake timing
There is currently no way to prevent Type 1 diabetes, and management requires lifelong insulin therapy.

Type 2 Diabetes: The Progressive Condition
Cause and Mechanism
Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas fails to produce enough insulin. Unlike the sudden autoimmune destruction in Type 1, Type 2 diabetes typically develops gradually over many years.
Who It Affects
Type 2 accounts for about 90-95% of all diabetes cases. While traditionally associated with older adults, it is increasingly diagnosed in children and adolescents due to rising obesity rates. Risk factors include:
- Excess weight and obesity
- Sedentary lifestyle
- Family history of diabetes
- Age (risk increases after 45)
- History of gestational diabetes
- Race/ethnicity (higher rates in African Americans, Hispanic/Latino Americans, American Indians, and some Asian Americans)

Key Symptoms
Type 2 diabetes symptoms develop slowly and can be subtle:
- Increased thirst and urination
- Increased hunger
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Areas of darkened skin (acanthosis nigricans)
- Many people have no symptoms initially
Treatment Approach
Treatment for Type 2 diabetes follows a stepwise approach:
-
Lifestyle modifications: Often the first line of defense
- Regular physical activity (at least 150 minutes per week)
- Weight management
- Healthy eating patterns
-
Oral medications: Various classes of drugs that work to:
- Increase insulin production
- Improve insulin sensitivity
- Reduce glucose production by the liver
- Increase glucose excretion through urine
-
Injectable medications: Including GLP-1 receptor agonists which slow digestion and help lower blood glucose levels
-
Insulin therapy: May be needed if other treatments don't achieve target blood glucose levels
Unlike Type 1 diabetes, Type 2 can sometimes be prevented or put into remission through significant lifestyle changes, particularly in its early stages.
Key Differences at a Glance
| Feature | Type 1 Diabetes | Type 2 Diabetes | |---------|----------------|-----------------| | Cause | Autoimmune destruction of beta cells | Insulin resistance and progressive insulin secretion defect | | Onset | Typically rapid | Usually gradual | | Age at diagnosis | Usually childhood/young adulthood | Typically middle age or older (but increasing in youth) | | Body type | Any | Often associated with obesity | | Insulin production | Little to none | Usually present but insufficient | | Insulin therapy | Always required | Sometimes required | | Prevention | Not currently possible | Often preventable with lifestyle changes |

Living with Diabetes: The Daily Reality
Regardless of type, living with diabetes requires daily attention and care. Both types require regular monitoring of blood glucose levels, although frequency may differ. Both also benefit from regular physical activity, stress management, and consistent medical care.
The psychological impact of diabetes management shouldn't be underestimated. Diabetes distress—the emotional burden of managing a demanding chronic condition—affects many people with both types of diabetes.
Looking Forward: Advances in Treatment
Exciting developments continue to improve life for people with diabetes:
- Continuous glucose monitoring (CGM) systems that eliminate or reduce the need for fingerstick tests
- Advanced insulin pumps with automated insulin delivery features
- New medications with benefits beyond glucose control
- Research into immunotherapies for Type 1 diabetes
- Progress toward artificial pancreas technology

Conclusion
While both Type 1 and Type 2 diabetes share the common problem of elevated blood glucose levels, they differ significantly in their causes, development, and treatment approaches. Understanding these differences is crucial for proper management and for developing effective treatment strategies.
If you suspect you may have symptoms of either type of diabetes, don't delay seeking medical advice. Early diagnosis and treatment can prevent serious complications and improve quality of life.
References
American Diabetes Association. (2022). Standards of Medical Care in Diabetes—2022. Diabetes Care, 45(Supplement 1).
Atkinson, M. A., Eisenbarth, G. S., & Michels, A. W. (2014). Type 1 diabetes. The Lancet, 383(9911), 69-82.






