The Science Behind Your Sugar Crash
We've all experienced it—that sluggish, foggy-headed feeling after indulging in birthday cake, holiday cookies, or that irresistible ice cream sundae. While we often attribute this sensation to guilt or simply "too much of a good thing," what you're actually experiencing has a scientific name: a sugar hangover. And yes, it's just as real as its alcohol-induced cousin.
As someone who has studied metabolic health for years, I can tell you that these symptoms aren't just in your head. They represent a genuine physiological response to rapid blood glucose fluctuations. The sugar hangover follows a distinct two-phase pattern that creates the perfect storm of physical discomfort.
Phase 1: The Spike (Postprandial Hyperglycemia)
When you consume refined carbohydrates or pure sugar—especially without the buffering effects of fiber, protein, or fat—glucose floods your bloodstream quickly. Your body, designed to maintain glucose within a narrow range, responds by triggering your pancreas to release insulin, the hormone responsible for ushering glucose into cells. This initial phase can leave you feeling temporarily energized, even euphoric.
Phase 2: The Crash (Reactive Hypoglycemia)
Here's where things go awry. The rapid insulin response that helped manage the initial glucose spike often overcorrects, sending your blood sugar plummeting below baseline levels. This reactive hypoglycemia typically occurs 2-4 hours after the initial sugar consumption, manifesting as:
- Sudden fatigue and weakness
- Irritability or mood changes
- Headaches
- Brain fog or difficulty concentrating
- Shakiness or trembling
- Increased hunger or cravings
- In some cases, anxiety or heart palpitations
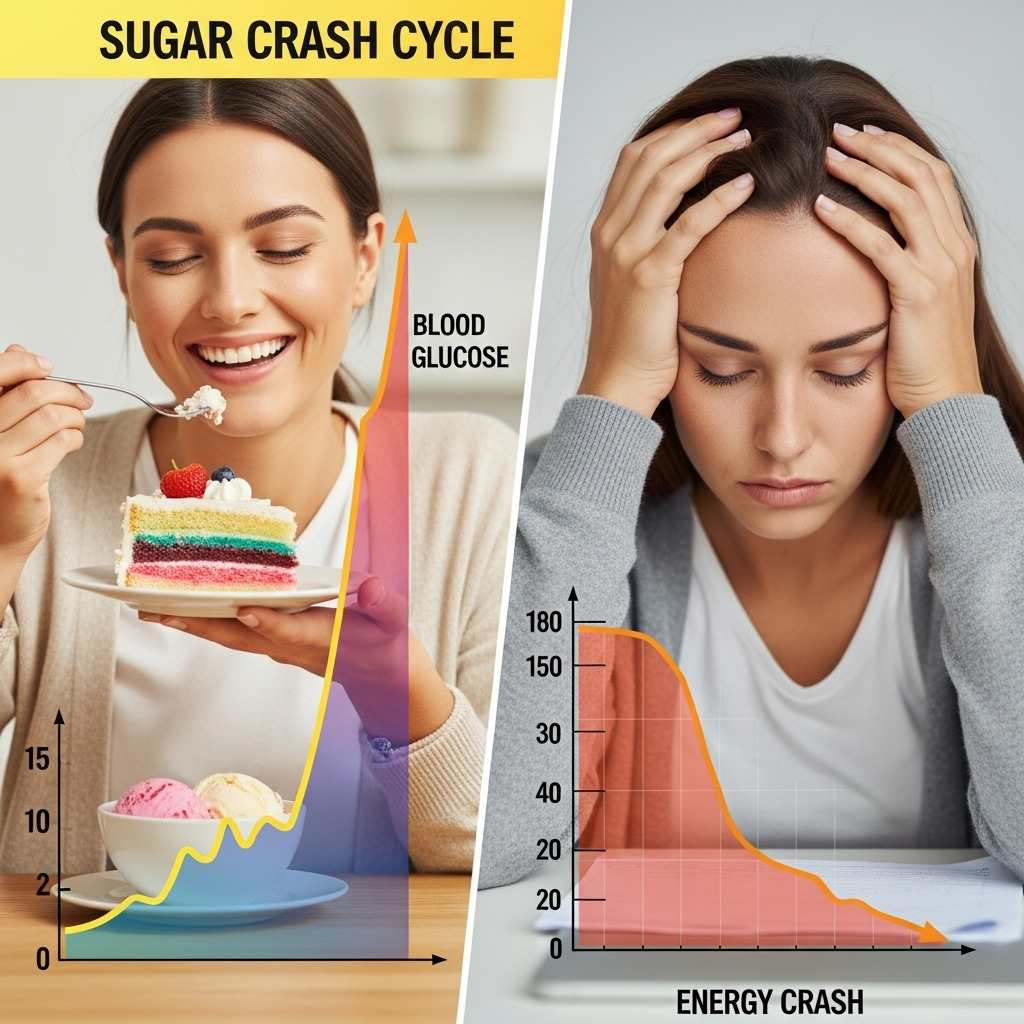
What makes this process particularly insidious is that these symptoms often lead us to reach for more quick-acting carbohydrates, perpetuating the cycle of spike and crash.
Beyond Discomfort: The Long-Term Consequences
While occasional sugar hangovers might seem like a mere inconvenience for metabolically healthy individuals, there's growing evidence that repeated glycemic roller coasters can have serious long-term implications.
For Those With Diabetes or Insulin Resistance
If you're among the estimated 122 million Americans with diabetes or prediabetes, these glucose excursions are more than uncomfortable—they're potentially dangerous. Glucose variability (the degree to which blood sugar levels swing throughout the day) has emerged as an independent risk factor for diabetes complications, even when average glucose levels appear controlled.
Even for "Metabolically Healthy" Individuals
Perhaps more concerning is what happens to those who consider themselves metabolically healthy. Research increasingly suggests that repeated glucose spikes followed by crashes—even without a diabetes diagnosis—may contribute to:
- Gradual development of insulin resistance
- Increased inflammation throughout the body
- Endothelial dysfunction (damage to blood vessel linings)
- Greater oxidative stress
- Accelerated cognitive decline
- Heightened risk of cardiovascular disease
- Weight gain and obesity
The mechanism is relatively straightforward: each significant glucose excursion creates a cascade of oxidative stress and inflammatory responses. Over time, these repeated insults can damage tissues throughout the body—from blood vessels to brain cells—potentially accelerating aging and disease processes.
This is why I often tell my patients and readers that glucose stability may be just as important as average glucose levels. It's not just about your A1C or fasting glucose, but how dramatically your blood sugar fluctuates throughout the day.
Strategic Approaches to Prevent Sugar Hangovers
The good news? You don't have to eliminate all sweetness from your life to avoid these unpleasant crashes. With some strategic approaches, you can enjoy occasional treats while minimizing the metabolic fallout.
1. Reimagine Your Relationship with Added Sugars
The average American consumes about 17 teaspoons of added sugar daily—far exceeding the American Heart Association's recommended limit of 6 teaspoons for women and 9 for men. Start by identifying and limiting the major sources of added sugars in your diet:
- Sugar-sweetened beverages (including juice)
- Processed snack foods
- Many breakfast cereals
- Flavored yogurts
- Condiments and sauces
- Pastries and desserts
2. Strategic Sequencing: When You Do Indulge
The order in which you eat foods can significantly impact glycemic response. When enjoying something sweet:
- Consume it after protein, fiber, and healthy fats, ideally as dessert following a balanced meal
- The fiber, protein, and fat will slow gastric emptying and glucose absorption, blunting the spike
- Consider starting meals with vegetables or a small salad with olive oil to prime your digestive system for better glucose responses

3. The Alcohol-Sugar Double Whammy
The combination of alcohol and sugar can create particularly severe crashes for several reasons:
- Alcohol inhibits gluconeogenesis (your liver's ability to produce glucose when levels fall)
- Many alcoholic beverages contain significant amounts of sugar themselves
- Alcohol can enhance insulin secretion, potentially worsening reactive hypoglycemia
- The dehydrating effects of alcohol compound symptoms like headache and fatigue
If you choose to consume alcohol, opt for lower-sugar options and be especially mindful of consuming adequate protein and fat beforehand.
4. Tactical Tools to Blunt Glucose Excursions
Several evidence-based strategies can help minimize glucose spikes when you do consume carbohydrates:
- Pre-meal activity: Even a 10-minute walk before or after eating can significantly reduce postprandial glucose spikes
- Vinegar before meals: One tablespoon of vinegar (in water or salad dressing) before a carb-heavy meal can reduce glucose response by 20-30%
- Adequate hydration: Proper hydration supports insulin sensitivity and helps your kidneys excrete excess glucose
- Strategic fiber: Adding soluble fiber (like chia seeds, flaxseeds, or psyllium husk) to higher-carb meals slows glucose absorption
- Stress management: Acute stress releases cortisol, which can elevate blood glucose independently of diet
5. Navigating a Sugar Crash in Progress
If you're already experiencing reactive hypoglycemia symptoms, your response should be calibrated to severity:
- For mild symptoms: Consume a balanced snack containing protein, fat, and complex carbohydrates (like apple slices with almond butter or hummus with vegetables)
- For moderate symptoms: Consume approximately 15 grams of fast-acting carbohydrates (like 4 ounces of juice or a small piece of fruit), followed by protein and fat
- For severe symptoms (confusion, inability to swallow, loss of consciousness): This requires immediate medical attention and is rare in non-diabetic individuals
Finding Balance in an Unbalanced Food Environment
Understanding sugar hangovers doesn't mean you must abstain from all life's sweet pleasures. Rather, it's about developing awareness of how your body responds to different foods and making informed choices that allow you to enjoy treats without the subsequent crash.
In our modern food environment, where hyperpalatable, ultra-processed foods dominate, maintaining stable blood glucose requires intentionality. However, with the right strategies, you can navigate special occasions and occasional indulgences while preserving metabolic health.
The goal isn't perfection but resilience—creating a metabolic system robust enough to handle occasional glucose excursions without falling into the chronic spike-and-crash cycle that underlies so many modern diseases.
By understanding the science behind sugar hangovers and implementing these practical strategies, you can enjoy greater energy, clearer thinking, more stable moods, and perhaps most importantly, build a foundation for long-term metabolic health that will serve you for decades to come.
References:
-
Ludwig DS, Aronne LJ, Astrup A, et al. The carbohydrate-insulin model: a physiological perspective on the obesity pandemic. Am J Clin Nutr. 2021;114(6):1873-1885. doi:10.1093/ajcn/nqab270
-
Ceriello A, Monnier L, Owens D. Glycaemic variability in diabetes: clinical and therapeutic implications. Lancet Diabetes Endocrinol. 2019;7(3):221-230. doi:10.1016/S2213-8587(18)30136-0






