Inflammation and Blood Sugar: The Hidden Connection Sabotaging Your Metabolic Health
In the quest for optimal metabolic health, we often focus on obvious factors like diet, exercise, and medication. However, there's a silent disruptor that deserves far more attention: inflammation. As someone deeply invested in understanding the complex relationship between our body's systems, I've come to recognize inflammation as a critical piece of the diabetes puzzle. Let's explore how this underlying process may be quietly derailing your blood sugar control efforts.
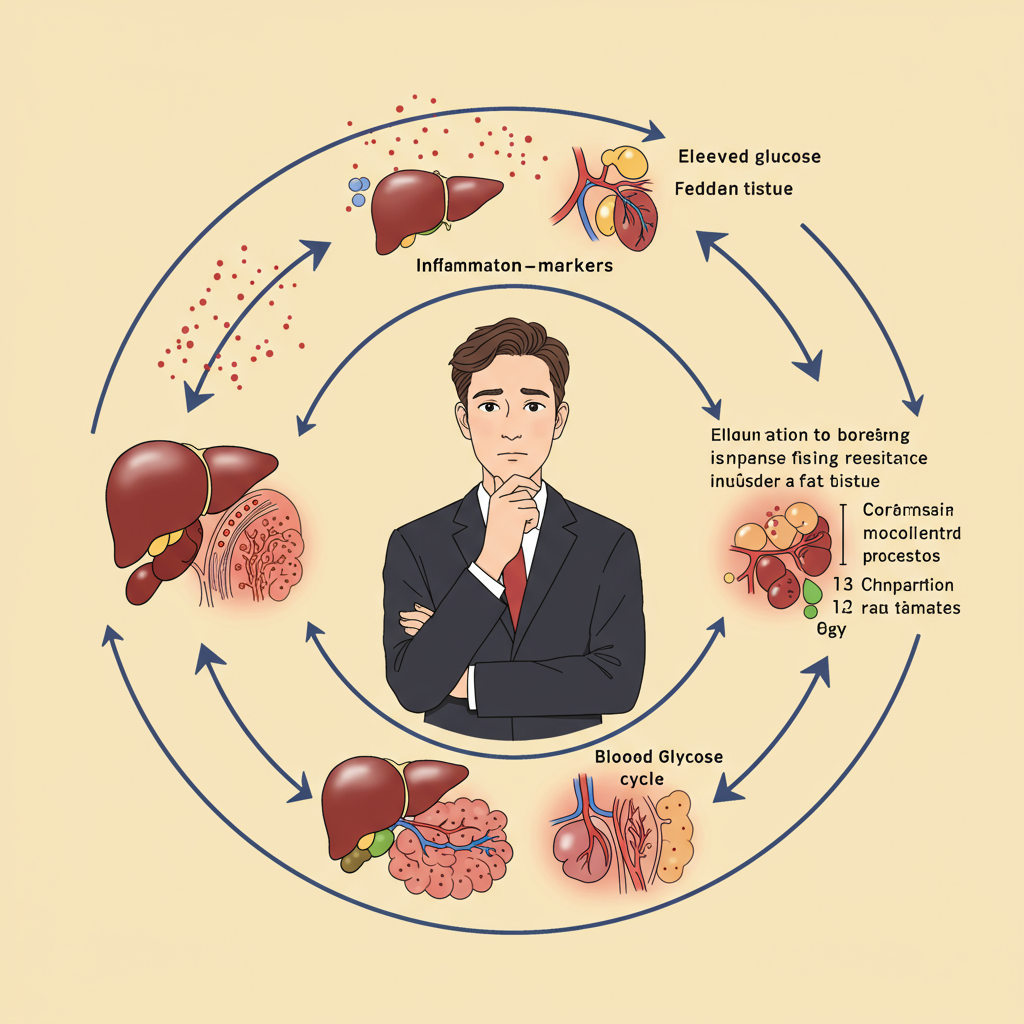
The Inflammatory-Metabolic Cycle: A Dangerous Feedback Loop
Inflammation and dysregulated blood sugar exist in a troubling reciprocal relationship. Chronic inflammation can trigger insulin resistance, while elevated blood glucose can amplify inflammatory processes. This creates a self-perpetuating cycle that becomes increasingly difficult to break.
At the cellular level, pro-inflammatory cytokines like TNF-α, IL-1β, and IL-6 interfere with insulin signaling pathways. These inflammatory messengers activate stress-response enzymes such as JNK and IKK, which phosphorylate insulin receptor substrate (IRS) proteins in a manner that blocks normal insulin action. The result? Your cells become increasingly deaf to insulin's signals, requiring your pancreas to produce more insulin to achieve the same glucose-lowering effect—the very definition of insulin resistance.
What's particularly concerning is how this process affects different tissues. In muscle, inflammation reduces glucose uptake. In the liver, it promotes excess glucose production. In fat tissue, it triggers the release of free fatty acids that further exacerbate insulin resistance. This multi-organ attack creates the perfect storm for metabolic dysfunction.
Beyond Obesity: Other Inflammatory Triggers Affecting Blood Sugar
While excess adiposity (particularly visceral fat) is a well-established source of inflammation, several other factors can trigger inflammatory processes that impact glucose regulation:
Gut dysbiosis: The composition of your gut microbiome significantly influences inflammatory status. Disruptions to the gut barrier can allow bacterial endotoxins (like lipopolysaccharides) to enter circulation, triggering systemic inflammation that promotes insulin resistance. This "metabolic endotoxemia" appears to be a key mechanism linking dietary patterns to metabolic health.
Psychological stress: Chronic stress activates inflammatory pathways through cortisol dysregulation and sympathetic nervous system activation. This explains why stress management isn't just good for mental health—it's essential for metabolic control.
Sleep disruption: Poor sleep quality or insufficient sleep duration increases inflammatory markers and impairs glucose metabolism, even in metabolically healthy individuals. Just one night of sleep deprivation can induce temporary insulin resistance.
Environmental factors: Exposure to certain environmental toxins, air pollution, and some medications can trigger inflammatory processes that compromise metabolic function.

Breaking the Cycle: Anti-Inflammatory Approaches to Blood Sugar Control
The recognition of inflammation's role in glucose dysregulation opens exciting avenues for intervention beyond traditional diabetes management. Here are evidence-based approaches to target the inflammatory component:
Nutritional strategies: Adopt an anti-inflammatory dietary pattern rich in omega-3 fatty acids, polyphenols, and fiber while minimizing refined carbohydrates, processed foods, and pro-inflammatory omega-6 oils. Specific foods with promising anti-inflammatory effects include fatty fish, extra virgin olive oil, berries, cruciferous vegetables, and fermented foods that support gut health.
Time-restricted eating: Condensing your daily food intake into a shorter window (typically 8-10 hours) may reduce inflammatory markers while improving insulin sensitivity, even without changing food choices.
Strategic exercise: While exercise has potent anti-inflammatory effects, the approach matters. High-intensity interval training appears particularly effective at reducing inflammatory markers while improving glucose control. However, excessive endurance training without adequate recovery can increase inflammation—moderation and recovery are key.
Targeted supplements: Several compounds show promise for addressing inflammation-induced metabolic dysfunction, including curcumin, resveratrol, and omega-3 supplements. Emerging evidence also supports the use of specific probiotic strains to modulate gut-derived inflammation.
Stress reduction: Incorporate evidence-based stress management techniques like meditation, deep breathing exercises, or cognitive behavioral therapy. The metabolic benefits of these practices likely stem partly from their anti-inflammatory effects.
The inflammation-blood sugar connection represents a paradigm shift in how we understand and treat metabolic dysfunction. By addressing the underlying inflammatory processes, we may finally break free from the frustrating plateau that many experience with conventional approaches to blood sugar management.
Remember, optimal metabolic health requires a comprehensive strategy that acknowledges this critical relationship between inflammation and glucose regulation. Your pancreas will thank you.

References
Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11(2):98-107. doi:10.1038/nri2925
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127(1):1-4. doi:10.1172/JCI92035






