When we talk about heart disease risk, most people immediately think of cholesterol numbers. But what if I told you there's a better predictor of cardiovascular risk that many doctors aren't routinely measuring? Enter ApoB (Apolipoprotein B-100) – a crucial marker that provides a more accurate assessment of your cardiovascular health than traditional cholesterol tests.
What Exactly is ApoB and Why Should You Care?
ApoB is a protein found on the surface of atherogenic lipoproteins – these include LDL (often called "bad" cholesterol), VLDL, IDL, and Lp(a). What makes ApoB special is that each of these potentially harmful particles contains exactly one ApoB molecule. This means ApoB gives us a direct count of all the particles that can potentially deposit cholesterol into artery walls.
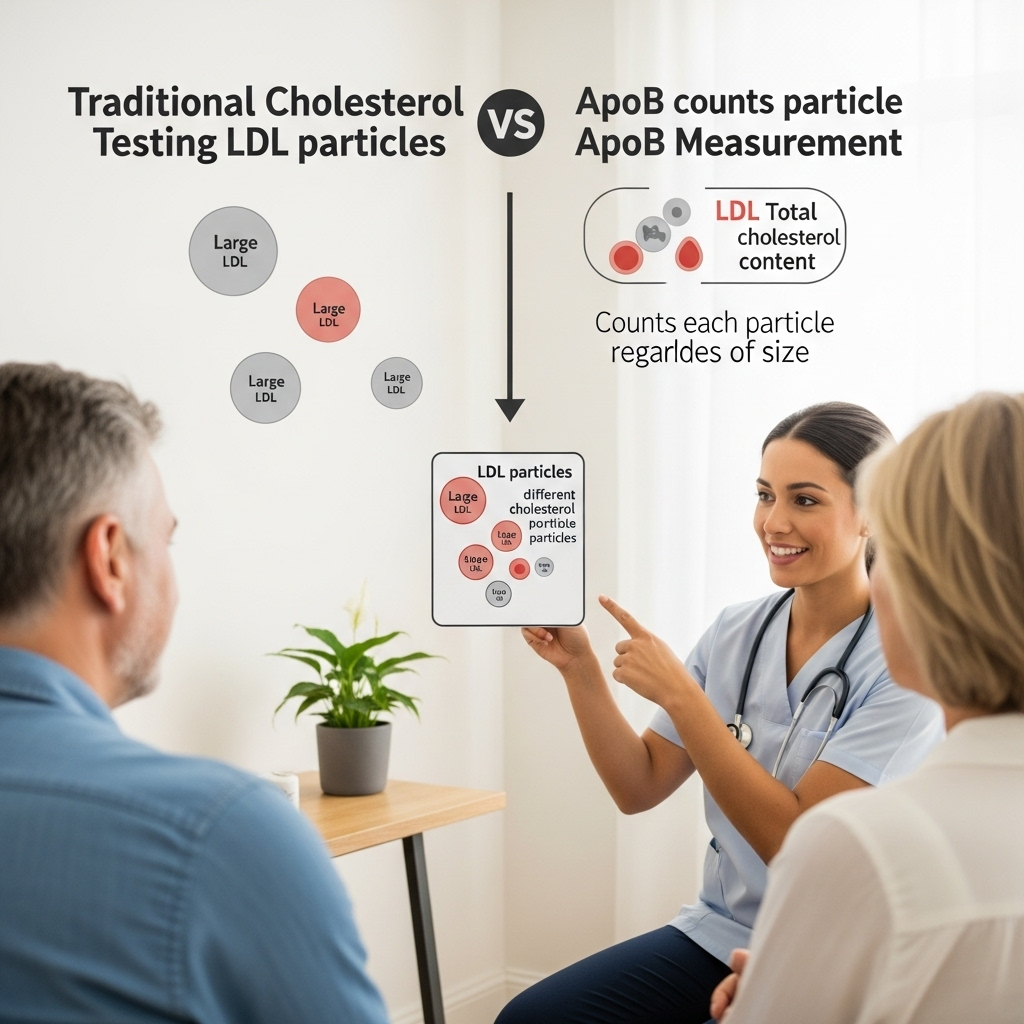
Think of it this way: Traditional LDL cholesterol tests measure the total amount of cholesterol in LDL particles, but they don't tell you how many particles are carrying that cholesterol. Two people could have identical LDL cholesterol levels, but one might have fewer large particles (lower risk) while another has many small, dense particles (higher risk). ApoB reveals this critical difference by counting all atherogenic particles.
This is why numerous studies have shown ApoB to be a superior predictor of cardiovascular events compared to LDL cholesterol alone. If you're serious about understanding your heart disease risk, ApoB deserves your attention.
What Are Optimal ApoB Levels?
Unlike some health markers where there's a broad "normal" range, with ApoB, lower is generally better. Here's what to aim for:
- General population: Below 90 mg/dL is considered desirable
- Higher risk individuals (those with diabetes, existing heart disease): Below 70 mg/dL
- Very high-risk individuals (multiple cardiac events): Below 60 mg/dL may be appropriate
Remember, these targets should be personalized based on your overall risk profile. Work with a healthcare provider who understands the importance of ApoB to determine your specific goals.

How to Improve Your ApoB Levels
The good news is that many strategies that benefit overall health also help reduce ApoB. Here's a comprehensive approach:
1. Dietary Modifications
-
Reduce refined carbohydrates and added sugars: High intake of poor-quality carbs increases triglycerides, boosting VLDL production and raising ApoB. Focus on complex carbohydrates with fiber.
-
Moderate saturated fat intake: Keep saturated fat below 7-10% of daily calories. Excessive saturated fat can decrease LDL receptor activity, making it harder for your body to clear these particles.
-
Increase omega-3 fatty acids: EPA and DHA from fatty fish or high-quality supplements can reduce VLDL production. Aim for at least two servings of fatty fish weekly or consider supplementation.
-
Boost soluble fiber: Beans, oats, barley, and fruits like apples contain soluble fiber that binds bile acids, increasing LDL clearance. Adding just 5-10g of soluble fiber daily can make a significant difference.

2. Exercise Strategically
Both aerobic exercise and resistance training can significantly improve your ApoB profile:
-
Aerobic exercise: At least 150 minutes of moderate-intensity activity weekly helps reduce ApoB and improves the ApoB:ApoA1 ratio (a powerful predictor of cardiovascular risk).
-
Resistance training: Adding 2-3 strength sessions weekly improves body composition and insulin sensitivity, both of which benefit ApoB levels.
The key is consistency – benefits accumulate with regular exercise over at least 12 weeks.
3. Medication Options (When Necessary)
If lifestyle modifications aren't sufficient to reach target levels, especially for high-risk individuals, medications can be valuable tools:
-
Statins: First-line therapy, reducing ApoB by approximately 19-42% by upregulating LDL receptors.
-
Ezetimibe: Decreases cholesterol absorption from the intestine, complementing statin therapy with additional ApoB reduction.
-
PCSK9 inhibitors: Powerful but more expensive option, reducing ApoB by 40-56% in clinical trials.
Remember that medication decisions should always be made in partnership with your healthcare provider, weighing individual benefits and risks.
Measuring and Monitoring Your ApoB
Request an ApoB test as part of your regular lipid panel. While not yet standard in all practices, more forward-thinking clinicians recognize its value. If your doctor doesn't offer it, explain why you believe it's important or seek a provider who includes this valuable marker in their assessment.
Your cardiovascular health is too important to rely on incomplete information. Understanding your ApoB level provides critical insight that traditional lipid panels might miss, allowing for more personalized risk assessment and treatment strategies.
References:
Sniderman AD, et al. "A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk." Circulation: Cardiovascular Quality and Outcomes. 2011;4(3):337-345.
Grundy SM, et al. "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol." Journal of the American College of Cardiology. 2019;73(24):e285-e350.






