Onkraj krvnega sladkorja: Razumevanje kritičnega prepletanja krvnega tlaka in holesterola pri zapletih sladkorne bolezni
Obvladovanje sladkorne bolezni je pogosto močno osredotočeno na nadzor glukoze, vendar lahko ta osredotočenost povzroči, da spregledamo širšo sliko. Kot nekdo, ki že leta raziskuje področje presnovnih bolezni, sem začel ceniti, da optimalna skrb za sladkorno bolezen zahteva pristop z “metabolično trojico”: krvni sladkor, krvni tlak in holesterol. Danes želim raziskati, kako ti trije dejavniki delujejo skupaj in zakaj je njihovo sočasno obravnavanje najučinkovitejša strategija za preprečevanje uničujočih zapletov sladkorne bolezni.
Žilna ranljivost: Zakaj najprej trpijo krvne žile
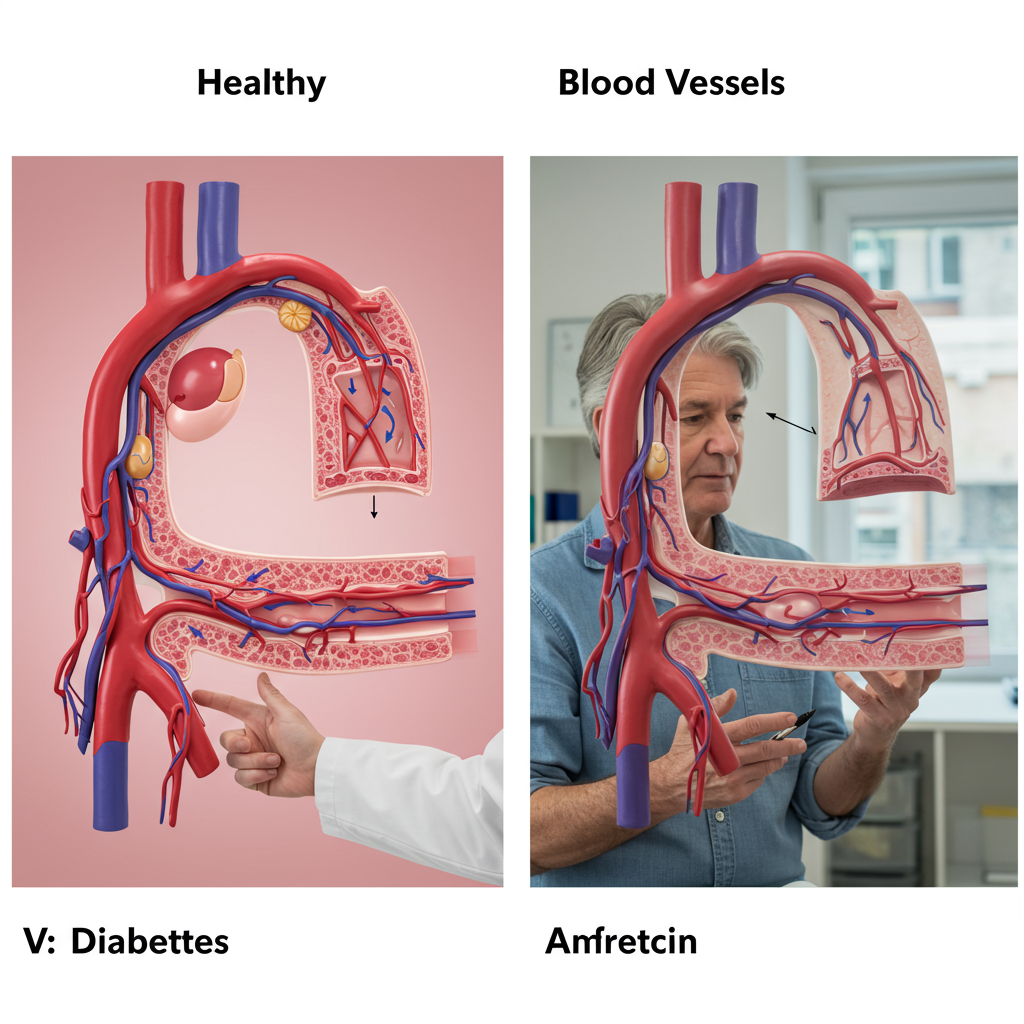
Kadar govorimo o zapletih sladkorne bolezni, dejansko govorimo o poškodbah krvnih žil. Hiperglikemija (povišan krvni sladkor) sproži to poškodbo, a hipertenzija in dislipidemija (nenormalni holesterol) jo dodatno pospešita in okrepita na različne načine.
Krvne žile se pri sladkorni bolezni srečujejo s popolnim viharjem škodljivih vplivov. Visok krvni sladkor sproži vnetje in oksidativni stres, ki poškodujeta endotelij – ključni notranji sloj krvnih žil. Ta endotelijska disfunkcija je prvi korak k aterosklerozi (strjevanju in zožitvi žil). Ko pa se pridruži še povišan krvni tlak, doda mehanski stres že oslabljenim žilam, dislipidemija pa vnese lipidne delce, ki lahko prodrejo skozi poškodovane stene žil in pospešijo nastanek plakov.
Ta sinergistična poškodba se pojavi tako v večjih žilah (makrožilni zapleti, kot so srčni napadi in kapi) kot tudi v manjših žilah (mikrožilni zapleti, ki prizadenejo oči, ledvice in živce). Dokazi so jasni: bolniki s sladkorno boleznijo, ki imajo nenadzorovan krvni tlak in holesterol, imajo eksponentno večje tveganje za zaplete kot tisti z zgolj hiperglikemijo.
Multiplikativni učinek: Kako se združujejo trije dejavniki tveganja
Odnos med temi tremi dejavniki ni le sešteven – je množenjski. Študija UKPDS je pokazala, da je bila za vsako odstotno točko znižanja HbA1c mikrožilna zapletenost manjša za 35 %. Ko pa so temu dodali še nadzor krvnega tlaka, je bilo zmanjšanje tveganja še precej večje.
Poglejmo nekaj številk, ki ponazarjajo ta multiplikativni učinek:
- Sama sladkorna bolezen poveča tveganje za srčno-žilne bolezni približno 2-krat
- Sladkorna bolezen + hipertenzija poveča tveganje približno 4-krat
- Sladkorna bolezen + hipertenzija + dislipidemija poveča tveganje približno 8-krat
Zaradi tega je večplastna intervencija bistveno učinkovitejša od zgolj glikemičnega nadzora. Prelomna študija Steno-2 je pokazala, da je intenzivna terapija, ki cilja na vse tri dejavnike, zmanjšala tveganje za srčno-žilne dogodke za približno 50 %, mikrožilne zaplete pa za 60–70 % v primerjavi s konvencionalnim zdravljenjem.
Posebej zanimivo je, da ti dejavniki tveganja skupaj ne nastajajo po naključju – imajo skupne patofiziološke korenine v inzulinski rezistenci in presnovnih motnjah. Inzulinska rezistenca povzroča ne le motnjo v uravnavanju glukoze, temveč prispeva tudi k hipertenziji skozi večje zadrževanje natrija in žilno disfunkcijo, hkrati pa spodbuja dislipidemijo, za katero so značilne visoke vrednosti trigliceridov, nizek HDL in majhni, gosti delci LDL.
Terapevtski pristop: Preseganje glukoznega centrizma
Ob upoštevanju teh dejstev mora naš pristop k sladkorni bolezni preseči zgolj nadzor glukoze. Tako izgleda celosten pristop:
Nadzor krvnega tlaka:
- Cilj: Na splošno <130/80 mmHg za večino ljudi s sladkorno boleznijo
- Pristop: Zaviralci RAAS (ACE-inhibitorji ali ARB) so posebej koristni zaradi dodatnih zaščitnih učinkov na ledvice
- Življenjski slog: Omejitev vnosa natrija, redna telesna dejavnost in obvladovanje stresa so temeljni ukrepi
Nadzor lipidov:
- Cilj: LDL-C <100 mg/dl (ali <70 mg/dl pri bolnikih z ugotovljeno srčno-žilno boleznijo)
- Pristop: Statini so še vedno terapija prve izbire, dokazi kažejo, da zmanjšajo srčno-žilne dogodke za 25–30 % pri ljudeh s sladkorno boleznijo
- Naprednejši vidiki: Število in velikost delcev pomenita več kot tradicionalne vrednosti holesterola; majhni, gosti delci LDL predstavljajo večje tveganje

Integriran pristop: Zdravila, ki izkazujejo največje srčno-žilne koristi pri sladkornih bolnikih (zaviralci SGLT-2 in agonisti GLP-1 receptorjev), delujejo deloma tako, da vplivajo na več dejavnikov tveganja hkrati. Zaviralci SGLT-2 na primer znižujejo krvni sladkor, hkrati pa zmanjšujejo krvni tlak in zagotavljajo neposredno karidiovaskularno in ledvično zaščito prek mehanizmov, ki jih še raziskujemo.
Zaključek: Pot naprej
Dokazi so nedvoumni: nadzor krvnega tlaka in holesterola ni drugotnega pomena glede na nadzor glukoze – je enako bistven. Za bolnike, ki jih skrbi pričakovana življenjska doba in kakovost življenja s sladkorno boleznijo, je celosten pristop, usmerjen v vse tri dejavnike hkrati, najboljša zaščita pred zapleti.
Dobra novica je, da številni ukrepi življenjskega sloga, ki pomagajo pri nadzoru krvnega sladkorja – sredozemska prehrana, redna telesna dejavnost, obvladovanje stresa in zadosten spanec – pozitivno vplivajo tudi na krvni tlak in holesterol. V kombinaciji z ustrezno farmakoterapijo, prilagojeno posameznikovemu profilu tveganja, tak celosten pristop predstavlja najboljšo politiko za razorožitev tega, čemur pravim “metabolična časovna bomba” sladkorne bolezni.
Ne pozabite: pri obvladovanju sladkorne bolezni nadzor glukoze pride v ospredje, a nadzor krvnega tlaka in holesterola rešuje življenja.

Viri:
-
Gaede P, Vedel P, Larsen N, idr. Večplastni pristop in srčno-žilne bolezni pri bolnikih s sladkorno boleznijo tipa 2. N Engl J Med. 2003;348(5):383-393. doi:10.1056/NEJMoa021778
-
UK Prospective Diabetes Study Group. Strog nadzor krvnega tlaka in tveganje za makrožilne in mikrožilne zaplete pri sladkorni bolezni tipa 2: UKPDS 38. BMJ. 1998;317(7160):703-713. doi:10.1136/bmj.317.7160.703






